Can a Dentist Break Your Jaw? My First-Hand Guide to Risks, Symptoms, and What to Do
Table of Contents
- Direct Force and Leverage
- Pre-Existing Jaw Conditions and Higher Risks
- Specific Dental Procedures With Greater Risk
Introduction: Why This Topic Matters to Me (and You)
I still remember when my friend nervously asked, “Can a dentist break your jaw?” She was about to get her wisdom teeth out, and she found scary stories online. That worry is pretty common. To be honest, before I got some dental treatments myself and talked to people in the field, I wondered about it too.
One thing I learned: knowing the facts helps more than worrying. When you understand how this happens, why it’s so rare, and what you and your dentist can do, it’s a lot less scary. I want to share what I’ve learned—both from my own visits and from talking with real dental workers.
Can a Dentist Really Break Your Jaw? Rare but Possible
Let’s be clear: Yes, a dentist can break your jaw during a dental job, but it’s really rare. I’ve spoken with lots of dental pros, and most haven’t seen this even once. Here’s why that should help you feel better:
- Your jaw (mostly the lower part, called the mandible) is very strong.
- Dentists and oral surgeons study for a long time and know how the jaw works.
- New tools and x-rays keep the risk very low.
So, think of breaking your jaw at the dentist a bit like getting hit by lightning on a clear day. It can happen in theory, but you’ll probably never see it yourself.
How and Why Jaw Fractures Happen During Dental Procedures
Even though it’s rare, sometimes the risk does go up. Here’s how it can happen (and why it almost never does if people are careful):
Direct Force and Leverage
Most of the time, a broken jaw happens from too much force or using tools the wrong way during hard extractions. Dentists use tools to loosen tough teeth (especially wisdom teeth that won’t come out). If someone tries to pull a very stubborn tooth with a lot of strength, it can push the bone too far.
It’s kind of like trying to pull out a nail stuck deep in old wood—if you pull too hard, the wood can crack unless you’re gentle.
Pre-Existing Jaw Conditions and Higher Risks
Not all jaws are the same. I saw this firsthand after learning how your health can raise or lower your chance of a broken jaw. If you’re about to have dental surgery, these things can add risk:
- Osteoporosis/Osteopenia: Thinning bones are weaker. Common as you get older.
- History of Jaw Trauma or Surgery: If your jaw was hurt before, it’s more likely to break.
- Cysts, Tumors, or Infections: Spots that are already damaged are easier to break.
- Radiation Therapy: Past cancer treatment in the mouth can weaken jaws.
- Elderly Patients: As we age, bones get more brittle.
I once talked to an oral surgeon who always asks patients about illnesses, medicines, and any jaw injuries before doing risky dental work. It’s not nosy—it’s smart and safe.
Specific Dental Procedures With Greater Risk
Trouble almost never happens with a simple filling or cleaning. The riskiest times are:
- Difficult Wisdom Tooth Extractions: Especially lower wisdom teeth that haven’t come in all the way or are stuck.
- Extractions With Fused or Ankylosed Teeth: Some teeth are “stuck” to the bone.
- Too Much Force or Wrong Technique: If the dentist isn’t trained for a tough job, or doesn’t call a specialist when it’s needed.
What I learned: It’s not checkups, but hard extractions with a lot of force—often when someone tries too hard to get a difficult tooth out.
Signs and Symptoms: How I Learned What a Broken Jaw Feels Like
Let’s say you or someone you know just had dental work, but something feels totally wrong. How can you tell if your jaw might be broken?
From stories I’ve heard and my own tough extraction, here are common red flags:
- Sudden, Really Bad Pain: Not the usual soreness, but pain that hits hard and won’t stop.
- Big Swelling and Bruising: If your face balloons up quickly on one side, more than the dentist said to expect.
- Hard to Open/Close Your Mouth: Called trismus—you can’t open as far or your bite feels weird.
- Numb Lip, Chin, or Tongue: This is serious since there are big nerves in your jaw.
- Loose or Oddly Missing Teeth: If more teeth than just the one pulled are wiggling, that’s a bad sign.
- Grinding, Clicking, or Crunching Sounds: Not just regular popping—some people say it feels or sounds like “stuff is moving or crunching.”
- Crooked Face: If your jaw or chin suddenly looks uneven.
- Weird or Heavy Bleeding: More blood than you’d expect, and it won’t quit.
Most of the time, normal soreness or swelling after dental work gets better in a few days. But if you feel any of the above, and it doesn’t seem normal or is getting worse, don’t wait.
How Dentists Confirm a Jaw Fracture
If you’re worried about this, a real diagnosis is the thing that helps. Here’s what I’ve seen dental pros do:
Exam:
The dentist will check your bite—do your teeth line up? They feel the jaw for any steps, pain, or funny movement. They’ll ask about numbness, see if your mouth opens right, and if your teeth fit together normally.
X-Rays and Scans:
Modern imaging helps right away:
- Panoramic X-Ray (OPG): Shows the whole jaw.
- CT or CBCT Scan: Gives a 3D view, good for tricky cases or if nerves are close by.
- MRI: Less common, but might be used if there’s something odd with the jaw joint.
It’s amazing how fast these images can clear things up. Sometimes, what feels bad is swelling, not a broken bone.
Treatment and Recovery: My Experience and What to Expect
If you do have a broken jaw, what’s next? I’ve seen people mend well, but it takes patience.
Keeping the Jaw Still:
The goal is to hold things in place so your jaw can heal:
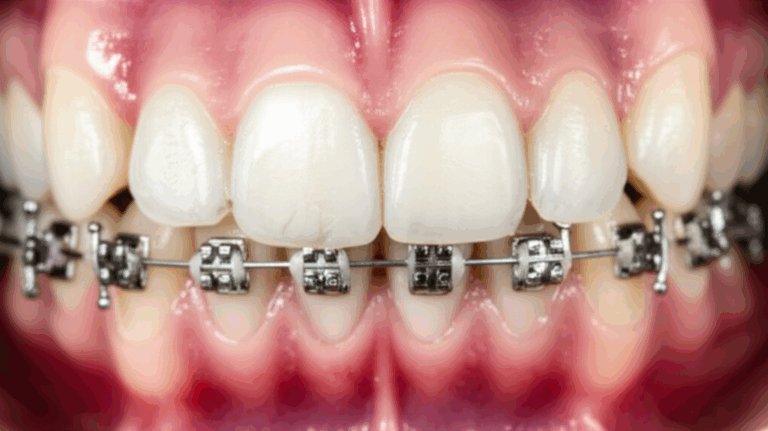
- Wiring the Jaws Shut (IMF): Teeth are tied together for a while.
- Splints/Arch Bars: These are little braces on your teeth to keep things lined up.
- Plates and Screws: If it’s a bad break, the surgeon might go in and “pin” the bone together, often from inside your mouth.
Caring for Yourself After:
- Pain relief: Medicine you can buy yourself or get from the doctor.
- Antibiotics: If needed to stop infection.
- Keep Your Mouth Clean: Super important since normal brushing may be hard.
- Food: Mostly soft stuff or liquids for weeks. Yes, you’ll get tired of soup and shakes.
- Jaw Exercises: Gentle moves after healing starts so you return to normal eating and talking.
It can take a few weeks to a couple of months to heal. The bright side? Most patients heal well if things are fixed quickly.
Steps to Take If You Suspect Your Jaw is Broken
Here’s what I always tell people (and did myself if I thought something was wrong):
Minimizing Risk: What I Do (and What Dentists Should Do)
Over time, I’ve learned some habits to keep safe—and I tell everyone to follow them, especially before big dental work:
If You’re the Patient:
- Share Your Health Info: Things like osteoporosis, certain medicines, or old jaw injuries matter a lot.
- Ask Questions: What’s the risk? How can we make it smaller? Should I see a specialist?
- Pick a Pro for Tough Jobs: If the tooth is stubborn (like a wisdom tooth), it’s ok to ask for a referral to an oral surgeon.
If You’re a Dentist or Assistant:
Here’s what great dental workers do:
- Look Closely at the Jaw First: Don’t just dig in—use x-rays and scans to spot trouble.
- Know When to Send to a Specialist: No dentist should be ashamed to send a tricky job to an oral surgeon.
- Use Gentle Force: No old-school yanking.
- Talk Openly About Risks: Telling the patient rare things that could go wrong helps build trust.
If you’re looking into work like crowns and bridges, dental implants, or big makeovers, ask how your clinic teams up with good labs and specialists for safe results.
Hard Numbers: Real-World Data and Case Studies
Let’s set the record straight with numbers. Keep in mind, these stats are tricky since doctors don’t always report “dentist broke jaw” directly. Here’s what I found from studies and talking with dental experts:
| Data Point | Key Facts |
|---|---|
| How Often Do Jaws Break After Teeth Out? | About 0.003% to 0.004% of all extractions. That means maybe a few out of tens of thousands. |
| Highest Risk Procedures | Lower wisdom tooth (bottom back teeth) extractions are the most risky for this problem. But most dentists never see it. |
| Who’s Most At Risk? | Older people, those with weak bones, those who’ve had jaw problems before, and those on special drugs. |
| When Do Symptoms Start? | Almost everyone knows within hours to a couple days—pain, swelling, and bite problems show up quick. |
| Healing and Results | If treated right, most people heal in 6-8 weeks. Very few have lasting trouble, and most problems come when treatment is put off or missed. |
| Suing or Complaints | Some people do report these cases, but winning money is rare unless the dentist was clearly careless. |
Example: I chatted with someone who had a lower wisdom tooth pulled. A few days later, she noticed more swelling, pain, and some numbness—her surgeon got a quick x-ray. Good news: no break, just a bad inflammation! Shows why being watchful and asking for help pays off.
Final Thoughts: Reassurance Backed by Experience
If there’s one thing I’ve learned, it’s that not knowing makes fear worse. When it comes to the question, “can a dentist break your jaw,” the facts are simple: it can happen, but it’s very rare, and it usually comes from hard extractions or hidden health problems.
Here’s what you can do:
- Pick your dental office wisely—ask about their experience with tough jobs.
- Don’t leave out your health info, even if it seems small.
- Say something if you feel wrong after your visit.
- Trust modern x-rays and care: even if you do break your jaw, quick action usually means a full recovery.
I’ve seen the best digital dental labs and oral surgeons work together to avoid problems and give people peace of mind. Your job? Be informed, be alert, and choose clinics that make safety number one.
If you ever worry “what if,” you’re not alone—and with the info here, you’re ahead of most people.
If you’ve got any questions, want to share your story, or still have worries, reach out or talk to your dentist. Honest talk is your first step to feeling safe.