What Anesthesia Do Dentists Use? My Simple Guide to Pain-Free Dental Care
Table of Contents
- Local Anesthesia: The Standard Numbing Experience
- Sedation Dentistry: Calming the Nerves
- Nitrous Oxide (Laughing Gas)
- Oral Sedation
- IV Sedation
- General Anesthesia: “Sleep Dentistry” for Bigger Needs
- Topical Anesthesia: The Numbing Gel Trick
- Is Dental Anesthesia Safe? My Honest Take
- Potential Side Effects and Complications
- Following Pre- and Post-Procedure Instructions
Introduction: My Journey to Understanding Dental Anesthesia
If you’ve ever walked into the dentist’s office with hands sweating, you’re not alone. For a long time, just thinking about sitting in the dentist’s chair made my heart beat fast. But things changed when I started to ask, “What kind of anesthesia do dentists really use, and how does it work?” That question opened a door to a world where pain doesn’t have to be part of your dentist story—and fear doesn’t have to run your whole visit.
In this guide, I want to break down everything I figured out (sometimes by making mistakes myself) about dental anesthesia. From my first trip that had way more fear than pain, to recent ones where I felt totally in charge, this article talks about what kinds of anesthesia dentists use, why, what they feel like, and how you can work with your dentist to pick the right one for you.
Why Dentists Use Anesthesia: It’s Not Just About Pain
Goals of Dental Anesthesia
When I first asked a dentist why anesthesia was such a big deal, it wasn’t just about pain. Here’s what I found out:
- Pain Control: Dental work can hurt, like fillings or getting wisdom teeth taken out. Anesthesia makes sure you don’t feel it.
- Less Anxiety and Fear: For people like me (and maybe you) who are nervous at the dentist, anesthesia really helps. It can even make folks with serious fear more comfortable.
- Helps Dentist Work Better: If I’m not jumping or tensing up, my dentist can do their job better, whether it’s a normal cleaning or a tricky treatment, like what’s made possible in a digital dental lab.
- Letting the Dentist Get Things Done: Sometimes dentists need you to be still and well, anesthesia—especially the sleepy kinds—makes that a lot easier.
What Influences Anesthesia Choice
I’ve noticed that dentists don’t just pick any old anesthesia every time. They think about a few things:
- Type and Time of Procedure: Tiny filling? Local numbing. Big surgery? Maybe sedation or even full sleep anesthesia.
- My Health and Allergies: I always tell them about my meds and allergies. That way they pick the safest thing for me.
- Anxiety: Some need a little calming, some (like my friend who’s super scared of the dentist) need heavier stuff or “sleep dentistry.”
- Kids and People with Special Needs: Young kids and people with some health problems may need a different kind of anesthesia.
Types of Anesthesia Dentists Use—What I’ve Seen and Felt
Local Anesthesia: The Standard Numbing Experience
Most of my dentist visits start with a little pinch and, soon after, that part of my mouth is numb. Here’s what’s going on:
- What It Is: Local anesthesia turns off nerves in one small spot, so I’m awake but I don’t hurt.
- Common Drugs: I usually hear names like Lidocaine, Articaine, Mepivacaine, and Bupivacaine.
- When It’s Used: Fillings, crowns, root canals, simple tooth pulling, and deep cleanings all use local.
- Good Stuff: It works quick, goes away in a couple hours, and does not mess up the rest of my body.
- Downside: My lip or cheek might feel weird and numb for 1–3 hours.
By the way, if you wonder how a dental filling or crown gets made after your tooth is numb, have a look at how a crown and bridge lab helps your dentist fix your smile.
Sedation Dentistry: Calming the Nerves
When numbing isn’t enough—especially if you’re worried—dentists use sedation. I’ve tried these myself, so let me tell you about them.
Nitrous Oxide (Laughing Gas)
- How It Works: I wear a little mask and breathe in the mix. In a few minutes, I feel lighter, calmer, even like it’s kind of funny that I’m in the dentist’s chair.
- Who Needs It: Great for mild nerves or short appointments. It wears off quick and I could drive home.
- What I Noticed: First time I had it, I thought, “Why didn’t I try this sooner?” Everything felt easier and as soon as the mask was off, it was gone.
Oral Sedation
- How It Works: I swallowed a small pill from the dentist—usually something like Diazepam or Triazolam—one hour before the visit. The sleepiness was slow but strong, so someone else had to drive me home.
- Who Needs It: For more nerves or longer visits, this makes things much easier.
- What I Noticed: I barely remember what happened—which, for me, was a good thing. These pills keep you awake, but really calm.
IV Sedation
- How It Works: The calming medicine goes straight into a vein through a little needle. This is a lot deeper than a pill or laughing gas—sometimes they call it “twilight sleep.”
- Who Needs It: If you get very nervous, have a tough gag reflex, or lots to get done at once, IV sedation helps a lot.
- What I Noticed: The whole time someone was watching my pulse, breathing, and oxygen. Not every dentist does this, but oral surgeons and some dentists with special training can.
General Anesthesia: “Sleep Dentistry” for Bigger Needs
- How It Works: When I had general anesthesia, I was all the way out—no clue what was going on.
- Who Needs It: Doesn’t happen much, but for big surgeries, super scared people, or kids who can’t stay still, general anesthesia is a safe choice when done by experts.
- Drawbacks: Waking up afterward takes longer and I needed someone with me before going home.
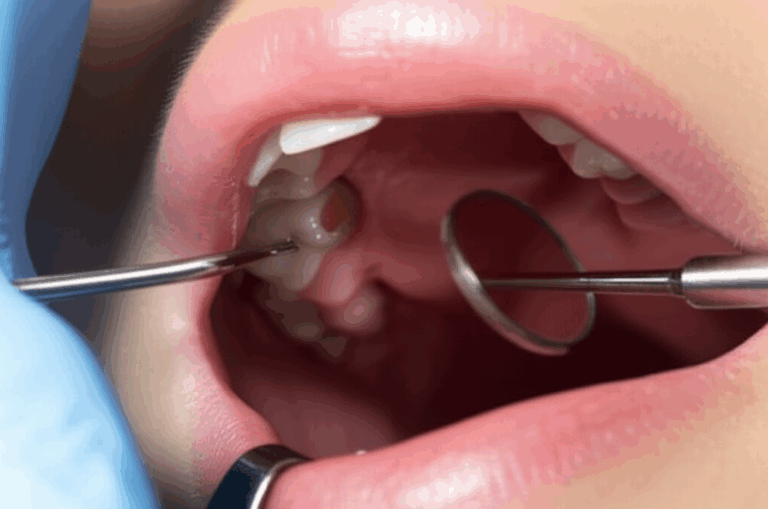
Topical Anesthesia: The Numbing Gel Trick
- What It Is: Before any needle, my dentist puts a strong numbing gel or spray on my gums.
- Why It Helps: This doesn’t numb like the shots do, but it makes getting a shot way less scary. It’s great for those who hate needles.
How I Help Choose the Right Dental Anesthesia
Let’s Talk About the Procedure
When my dentist and I talk about anesthesia, we look at the details together:
- Simple or Not: For a small cavity, local is fine. For pulling out a wisdom tooth, I might go for sedation—just to feel better about it.
- Short or Long: If I’ll be in the chair a while, I’m more likely to ask for something that keeps me relaxed, like a calming pill or IV drip.
Managing Your Anxiety—and Mine
If you’re like me, dentist nerves don’t just go away. Telling my dentist about my worries made all the difference. Here’s what I suggest:
- Speak Up: Tell your dentist what makes you worry. They’ve seen it before and want to help.
- Look at Options: Sometimes, just knowing you can pick—from laughing gas to IV sedation—makes you less scared.
- Plan Ahead: For a pill or IV, get ready: don’t eat if you’re told not to, and get a ride set up.
- Ask Questions: Wondering if your insurance pays for sedation? Ask early.
Safety, Risks, and Realistic Expectations
Is Dental Anesthesia Safe? My Honest Take
Don’t let spooky stories on the internet scare you. In my experience—and what dentists say—anesthesia for dental work is super safe when done by people who know what they’re doing. I believed it most after seeing all the safety steps in the office:
- Medical Check: A good dentist asks about my health, allergies, and any meds I take.
- Monitoring: For any deeper sedation, someone is watching my pulse and breathing the whole time.
Potential Side Effects and Complications
Here’s what I felt or saw—and what you might have too:
- Most Common: Numbness, puffy gums, maybe dizzy or sleepy for a bit.
- Less Common: Allergic reaction, upset stomach, or bigger problems (if you don’t tell your dentist about your health).
- Safety Numbers: Bad reactions to local numbing drugs like Lidocaine are less than 0.01%. Full sleep anesthesia is riskier but still almost never goes wrong for healthy people (less than 1 in 200,000).
Following Pre- and Post-Procedure Instructions
I once ate breakfast before a sedation appointment—bad idea. The dentist was not happy. Always:
- Don’t Eat if Told: For pills or IV jobs, your dentist might say ‘no food’ for a while before.
- Get a Ride: After sedation or sleep anesthesia, someone else should drive you home.
- Aftercare: You’ll feel numb, so skip hot drinks, watch for weird stuff, and follow your dentist’s advice.
FAQs: Your Most Pressing Dental Anesthesia Questions Answered
Q: How long does dental numbing (local anesthesia) usually last?
Most times, the numbing from a local shot lasts two to four hours. Some people feel tingly or a bit numb longer, depending on what’s used.
Q: Can I drive myself home after dental sedation?
With laughing gas, yes—I’ve done it lots of times. For pills or IV sedation, no—you need someone to drive you safely.
Q: What should I do if I’m afraid of needles at the dentist?
Say something! They’ve seen everything. Those numbing gels really work, and laughing gas helps you chill out before any shots.
Q: Is “Novocaine” still used by dentists today?
Novocaine was used long ago. Now, dentists use safer, longer-lasting stuff like Lidocaine, Articaine, or Mepivacaine.
Q: What’s the main difference between sedation and general anesthesia?
Sedation keeps me awake but calm; general anesthesia knocks me all the way out. Most dental visits only need sedation.
Q: Does dental insurance cover the cost of sedation?
It depends. Local numbing is covered most times. Sedation or general anesthesia might need a reason, and not every plan pays for it—ask about it first.
Statistics, Stories, and Surprises from the Dental Chair
Here’s some stuff I found out that really surprised me:
- Local anesthesia is used in over 95% of all routine dental procedures.
- About 30–50% of dental offices use laughing gas.
- Less than 5% have IV sedation in the office.
- True allergies to numbing drugs like Lidocaine almost never happen (<0.001%).
- Almost all patients (up to 95%) who try sedation say it helps a lot with their fear.
A friend of mine was really scared before getting dental implants. He picked IV sedation, and afterward, he was shocked at how easy it was. If you’re thinking of implants, think about which type of anesthesia helps you feel safe—especially when looking at places like an implant dental laboratory.
When I finally had a deep cleaning that I’d put off forever, laughing gas made it much easier than I thought it would be.
Conclusion: Your Path to Pain-Free, Anxiety-Free Dental Visits
If you’re like me, you want your dentist visits to be simple and not scary. What I learned—after years of trying, messing up, and asking questions—is that anesthesia changed dentistry in a big way. Now it’s not just about stopping pain; it’s about helping you (and me) feel calm and looked after.
Last bit of advice: Always tell your dentist about your fears, worries, or things that happened in the past. They want to help, and with all these ways to handle pain and fear, there’s a good choice for everyone.
Still feel nervous? Read more about different dental labs, like a china dental lab, and see how new dental technology keeps making visits smoother and less stressful.
Don’t let fear or worry keep you from a healthy, good-looking smile. Your best dentist visit is coming up—and trust me, it can be way easier than you think.
Thanks for reading my guide on dental anesthesia. If you have questions or want to share your stories, reach out—we can make dental care better for everybody.